Case-presentation: AYURVEDIC LINE OF TREATMENT IN RAKTAATISARA/RAKTAJA PRAVAHIKA (ULCERATIVE COLITIS)- A SINGLE CASE STUDY
**Vd. Anamika S. Soni
***Dr. Binjal Patel
****Dr. Kishan Senjaliya
ABSTRACT
Raktaatisara/Raktajapravahika(ulcerativecolitis) is condition of inflammation and ulceration
of lower intestinal mucosa causing recurrent melena & pain in abdomen.
Changing lifestyle, food habits, food adulteration, fast food etc. are main
causes for this disease. Contemporary modern science treats this condition with
antibiotics, anti-inflammatory and steroids etc. but there is no permanent
cure. Ayurveda is capable to provide complete cure easily with its specific individualized
classical approach, if patients directly approach to the Ayurvedic physician.
A
22-year old male patient with history of irregular life style and food habits,
presented with complaint of on & off abdominal pain, hyperacidity and melena
was successfully treated in Govt. Akhandanand Ayurveda College Hospital on the
basis of principles of classical Ayurveda and use of piccha vasti.
KEYWORDS: Colonoscopy, Raktatisara/Raktajapravahika, piccha
vasti
INTRODUCTION:
Ulcerativecolitis is a chronic idiopathic inflammatory bowel disease(IBD)[i]. InAyurveda, it canbe correlated with raktaatisara/raktajapravahika[ii]. Pittaatisara is one type of atisara described in Charaksamhita, it is caused by excessive use of pittavardhak aahara &vihara like- amla, tikshna, ushna, katu Pradhan rasa and kinva(fermented), use of kshara (soda bicarbonate) and other environmental causes like agni-suryasantap (excessive exposure of heat & sunlight), ushna marut uptap (excessive exposure of warm air or wind). it is also caused due to mansika vikara (disturbed mind) like- krodha(anger), irsya (jealousy) etc. When this type of lifestyle is continued with irregular food habits and sleep, mental stress etc. symptoms aggravate and further lead to the condition(phase) known as raktaatisara/raktajapravahika[iii].
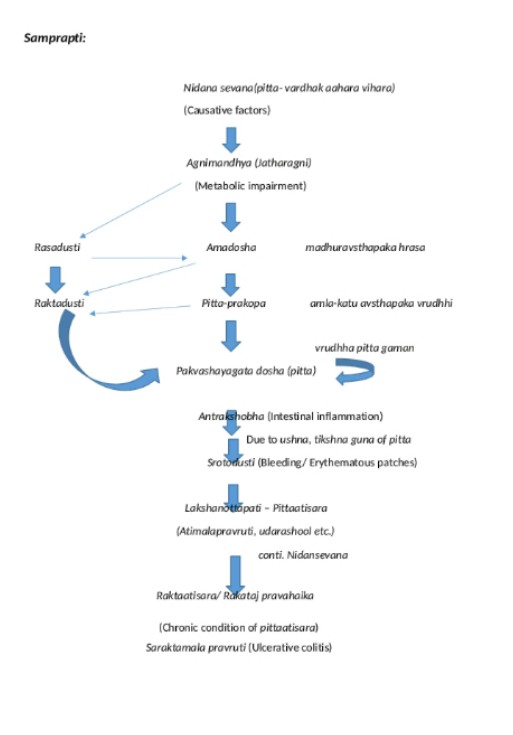
In Modern science, chronic raktajatisara condition clinically similar with ulcerative colitis. It is an idiopathic form of acute and chronic ulcero-inflammatory colitis affecting chiefly the mucosa and sub-mucosa of the rectum and descending colon. Though sometimes it may be involved the entire length of large bowel. There is prevalence rate of UC is about 44.3/100,000 and incidence of UC cases rate about 6.02%/100,000. In India about morethan 1.1 million People suffers from this disease. In this case, according to Ayurveda, we have tried to assess the samprapti ghataka (pathological agent), samprapti (pathophysiology) and made effort to break the vicious cycle of pathogenesis of the disease, leading to root eradication of the disease.
CHIEF COMPLAINTS:
>Abdominalpain(udarshool)- +++ Since 3 months
·>Foul smelling frothy diarrhoea with mucous
>Sakapha durgandhit Malapravruti)- +++ Since 3 months
B>Burning sensation on epigastric region(Urahadaha)- +++ Since 3 months
>Blood instool (Saraktamalapravruti)- +++ Since 1 week
>Anorexia(Aruchi)- +++ Since 1 week
>Weakness(Dorbalya)- ++ Since 1 week
>Frequent Stools- 6-7 times per day
He was diagnosed and treated in modern allopathy
hospital as a case of ulcerative colitis. According to his parents that he
stayed at home alone when they were out of station because of social cause. The
patient used to consume fast and junk food from market in routine and his
daily routine was very much disturbed and irregular.
Initially mild abdominal pain, heart burn, anal
burning etc. symptoms occurred
but patient continuously consumed vada-pav etc. junk food. When above symptoms occurred, he was
hospitalized, diagnosed and treated as a case of ulcerative colitis. Due to
side effects and patent modern drug toxicity, patient was brought to our hospital.
>Blood instool (Saraktamalapravruti)- +++ Since 1 week
>Anorexia(Aruchi)- +++ Since 1 week
>Weakness(Dorbalya)- ++ Since 1 week
>Frequent Stools- 6-7 times per day
He was diagnosed and treated in modern allopathy hospital as a case of ulcerative colitis. According to his parents that he stayed at home alone when they were out of station because of social cause. The patient used to consume fast and junk food from market in routine and his daily routine was very much disturbed and irregular.
Initially mild abdominal pain, heart burn, anal burning etc. symptoms occurred but patient continuously consumed vada-pav etc. junk food. When above symptoms occurred, he was hospitalized, diagnosed and treated as a case of ulcerative colitis. Due to side effects and patent modern drug toxicity, patient was brought to our hospital.
PAST HISTORY: No any specific
FAMILY HISTORY: Nil
PERSONAL HISTORY:
DIET: Veg, junk food, fast food
SLEEP: Irregular (Ratri jagarana)
APPETITE: Irregular
BOWEL MOVEMENT: 6-7 times/day
MICTURITION: 5-6 times/day, 1-2 times/night
PULSE: 80/min
BP: 120/80 mm/hg
R.R: 20/min
Temp: 98F
INVESTIGATIONREPORTS: COLONOSCOPY REPORT
DIAGNOSIS:
On the basis of clinical history, clinical presentation and colonoscopy investigation, patient was diagnosed as a case of Raktajaatisara/pravahika.
THERAPUTIC INTERVANTION[iv]:
Picchavasti was planned in themanagement, but patient refused to take vasti because of his exam. So, initially medicine (Shamanachikitsa) was started as below:
|
Medicine |
Dose |
Duration |
|
Rasayan tikdi |
2 tab.TDS |
30 Days |
|
Chandrakala Rasa |
2 tab.TDS |
30 Days |
|
Kutaja ghanavati |
2 tab.TDS |
30 Days |
|
2 tab.QID |
30 Days |
|
|
Tab. Posexforte |
2 tab.QID |
30 Days |
All these medicines given with plain water after meal.
The patient got some symptomatic relief with these drugs. After that patient was admitted in IPD for further picchavasti[v] for 14 days.S election of vasti dravyas was as per drug available in IPD. Vasti dravyas used in vasti was as below.
|
Doses |
|
|
Khadira churna |
10gm |
|
20gm |
|
|
Vasa churna |
10gm |
|
Guduchi churna |
20gm |
|
Arjuna churna |
10gm |
|
Lodhra churna |
10 gm |
|
Panchavalkala kwatha |
50gm |
|
Dugdha |
250ml |
Picchavasti (Ksheer based) was prepared as per ksheer paka vidhi and 300 ml. picchavasti was administered following modified drip method of vasti administration. Vasti was basically planned as Apunarbhava chikitsa.
Pathya–Apthya(wholesome diet and activity-
do’s &dont’s):
Patient was advised for pathyaaahara and vihara during the course of medication like–fresh home cooked, warm, easily digestible light diet like – khichadi (vilepi), mudgayusha (greengram soup), vegetables soups etc. Patient was barred for day sleep (divaswapa) and awakening at night (ratrijagarana), exposure with pravata (direct exposure of wind), forceful suppression of natural urges(vega).
ASSESSMENT OF DISEASE IMPROVEMENT:
SUBJECTIVECRIETERIA:
|
SYMPTOMS |
B.T. |
A.T. |
|||||
|
|
|
Pt. on oral medication (Shamana chikitsa) |
Pt. on picchavasti (Shodhana chikitsa) |
||||
|
|
|
1st week |
2nd week |
3rd week |
4th week |
1st week |
2nd week |
|
Abdominalpain (Udarshool) |
+++ |
+++ |
+++ |
++ |
+ |
+ |
- |
|
Foul smelling frothy diarrhoea withmucous (Sakaphadurgandhita malapravrutti) |
+++ |
+++ |
+++ |
++ |
++ |
+ |
- |
|
Burning sensation in epigastric region(Urahadaha) |
+++ |
+++ |
++ |
++ |
+ |
+ |
- |
|
Bloodinstool (Sarakta malapravrutti) |
+++ |
+++ |
+++ |
++ |
+ |
+ |
- |
|
Anorexia(Aruchi) |
+++ |
+++ |
++ |
++ |
++ |
+ |
- |
|
Weakness(dourbalya) |
++ |
++ |
++ |
++ |
++ |
+ |
- |
|
Stool frequency |
6-7 times/day |
6-7 t/d |
4-5 t/d |
3-4t/d |
1-2t/d |
1-2t/d |
1-2 t/d |
INVESTIGATION AFTER TREATMENT: COLONOSCOPY; DATE 15 DECEMBER 2021
RESULT:
After Vasti chikitsa patient got complete relief in all signs & symptoms with physical as well as mental wellbeing and cheerfulness in life.
FOLLOW-UP:
|
Medicine |
Anupana |
Dose |
|
Shatavari chu. – 5 gm Nagakesara chu. – 5gm Guduchi churna –3gm (ksheerpaka method) |
- |
2 times/day (Empty stomach) |
|
Samshamani vati |
Plain water |
2 tab. BD |
|
Amalaki chu.– 2 gm Dhatri loha–500 mg Mu.shukti B.500mg |
Honey |
1 tsf 2 times/day |
DISCUSSION:
Agni is the basic factor responsible for normal metabolic function. In pittaatisara, there is an increased in pitta gunas specially drava, ushna, sara, tikshna etc. when pittaatisari patient further indulge pittaj nidana then excessive increased said pitta gunas leading to reactive decreasedin dhaturupa shleshma and leads to erosion of intestinal mucosa and rupture of capillaries by ushna, tikshna pitta gunas. Increased sara guna lead to diarrhea and reactive vata prakopa is responsible for pain in abdomen etc. So, we can say that pitta is mainly responsible for the such clinical presentation. Raktaatisara/Raktapravahika presentas frequent stools with melena is main characteristicfeature. Patients with Pittaatisara have tendency to develop Raktaatisara when they donot follow pathyaahara-vihara and take hot, spicy, fried, junk food and fast food along with irregular life style leads to Raktaatisara as per the mechanism explained above, the samprapti ghataka (pathological agent) and samprapti (pathophysiology)as shown below. We made an effort to break the pathogenesis of the disease with basis of below samprapti and patient got complete relief with root eradication of the disease.
Samprapti ghatak:
1.Dosha:
Dravyatah vriddhi: Inflammation
Gunatah vridhhi: Ushna,
Tikshna, Sara, Drava Guna
Karmataha vridhhi: Diarrhea
∆ Pitta-vriddhi-
Pachak: -
Ranjak: +
Aalochak: -
Sadhak: -
Bhrajak:. +
∆ Vat-vriddhi-
Pran: ++
Udan: +
Saman: +++
Vyan: +
Apan: ++++
∆ Kapha-kshaya-
Kledak: ++++
Shleshak: -
Tarpak: -
Avalambak: +
Bodhak: +
2. Dushaya: Rasa, Rakta, Sweda, Mutra, Purisha
3. Srotasa: Annavaha, Udhakavaha, Swedavaha, Mutravaha, Purishvaha
4. Srotodusti prakara: Atipravruti
5. Rogamarga: Kostha
6. Agni: Vishama
7. Samata: Sama
8. Udabhavsthana: Aamashaya
9. Adhisthana: manodaihik
10. Vyaktisthana: Pakwashaya
11. Swbhava: Ashukari
12. Sadhya-asadhyta:Sadhya
Therefore, the first line of treatment is nidanaparivarjana followed by use of Rakta-stambhaka an dgrahi medicines.
The therapeutic plan was advised specifically as per the condition of patient and drugs availability in Govt. Akhandanand Ayurveda College Hospital. Chandrakala rasa and Rasayana tablet was advised as dosha pratyanika, Kutaja ghanvati and Posex forte tablet was advised as per vyadhi pratyanika, Livomyn tablet was added as a tikta, liver tonic and deepan drug. Vasti was selected as per instruction by acharya charak very similar to picchavasti and based on availability of drugs in IPD.
Vasti is a very unique therapeutic procedure that directly reaches at site of lesion and mainly acts with the rasa. It was modified as per the condition of patient and given with drip method, so vastidravyas could interact the lesion for longer duration in comparison to classical method. Tikta rasa has agood properties as shothanasak, kledahara, pittashamak, kapha-pittashoshan, ropana & sheeta. When it is processed in milk, it becomes highly effective as seen in this case. Vasti not only possesses local action but also it reaches the whole GIT and body because of its remote action. Tikta picchavasti is fully capable to cure the condition of vatasthangat pitta (as seen in UC) with principle of स्थानंजयेद्धि पूर्वंस्थानस्थस्याविरुद्धम्च[vi](cha.chi.23).
CONCLUSION:
Ulcerative colitis is now becoming a very big problem for medical fraternity specially in urban areas because of modern diet & life style and absence of root eradication treatment in modern science. The use of steroids progressively worsen the immunity of the patient leading to hazardous effects. Ayurveda provides apunarbhava chikitsa(root eradication treatment) with its specific classical approach.
[i] Api the textbook of medicine volume1 editor-siddharth N shah,8thedition.
[ii] Agnivesh charaka samhita vidyotini hindi commentary by pt. kashinatha shastri & dr. Gorakhanath chaturvedi published by chaukhambha bharti Academy, charaka samhita.
[iii] Sushrut samhita edited with ‘sushrutavimarsini’ hindi commentary by Anant ram sharma, chaukhambha surabhi prakashan, sushrutsamhinta.
[iv]
Bhaishajyaratnavali of shri govinddas, edited and enlarged by bhishagraj shri bhrahmashankar Mishra-vidhyotani hindi commentrary, chaukhambha prakashan edition:18threvised,2019.
[v]Sushruta Samhita edited with ‘sushrutavimarsini’ hindi commentary by Anantram sharma, Chaukhambha Surabhi prakashana, Sushruta Samhita
[vi]Agnivesha,
Charak, Dridbala, Charakasamhita, Visha chikitsa adhyaya-23/64 edited by Pt.
Kashinath Shastri and Dr. Gorakhnath Chaturvedi, edition 2018, Chaukhambha
Bharati Academy, Varanasi 2018;635pg
**************************************************************************************************************



Nice explanation
ReplyDelete