AYURVEDIC MANAGEMENT
OF CHRONIC PANCREATITIS
(JEERNA-PITTODAR)
*Dr. Nirali S. Thacker
**Prof. Surendra A. Soni
ABSTRACT
The case of chronic pancreatitis with Malabsorption Syndrome with presentation of diabetes mellitus was treated successfully with classical line of treatment of Pittodara chikitsa. In ayurveda we can corelate it with Pittodara. Treatment given includes the use of Kshirbasti, Deepana, Pachana, Anulomana, Srotoshodhana, Brinhana, Ksheer abhyasa etc. targeting to the basic site of pathology along with main site of pitta Dosha (Aamashya).
Pancreatitis
usually leads to Diabetes Mellitus and other consequences including malignancy
if not checked appropriately, while timely ayurveda management not only cure
the disease but also check the all its consequences that is mentioned in this
case study.
KEYWORDS :
Chronic pancreatitis, Malabsorption syndrome, Diabetes mellitus, Pittodara,
Pancreatic cancer, Kshirbasti, Deepana, Pachana, Anulomana,
Sroto-shodhana, Brinhana, Ksheer abhyasa, pitta dosha, Aamashya.
INTRODUCTION
The Pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. Pancreatitis is a condition characterized by inflammation of the pancreas. Pancreatitis is commonly described as autodigestion of the pancreas. There are two main types of clinical presentation:
acute pancreatitis
chronic pancreatitis.
Acute Pancreatitis is an acute inflammatory process of pancreas. The degree of inflammation varies from mild edema to severe hemorrhagic necrosis. Chronic pancreatitis is continuous, prolonged, inflammatory and fibrosing process of pancreas[i].
The
annual incidence of chronic pancreatitis is 5-12 per 100000 persons, the
prevalence is 50 per 1,00,000 persons[ii].The
two most common causes of acute pancreatitis are; (1) A gallstone blocking the
common bile duct after the pancreatic duct has joined and (2) heavy alcohol
use. Chronic pancreatitis may develop as a result of acute pancreatitis. In
chronic pancreatitis weight loss, steatorrhea, vomiting and diarrhea may occur[iii]. Complications
may include infection, bleeding, diabetes mellitus, Jaundice, pancreatic cancer
etc. As disease progresses defective autophagy, increased inflammation,
pancreatic stellate cell activation and fibrosis occur[iv].
According to Ayurveda Agnimandya is mentioned as basic etiological
factor for development of Udararoga. Intake of excessive hot, saline,
sour drinks, improper Samsarjana krama after Panchkarma therapy, Arsha,
Grahani and Plihadosha, presence of Ama, ulcerations and
perforations are the other causes described in our classics. Low and delayed
digestion, burning sensation, inability to determine between digestion and
indigestion, disappearance of folds with prominent network of veins over
abdomen occurs initially are some of the prodromal features of Udara-roga.
It has been described of eight types of Udar-rogas in Ayurveda[v].
We
can correlate pancreatitis as Pittodara in ayurveda. Pittodara
clinically presents with fever, burning sensation, thirst, diarrhea, fainting,
yellowish discoloration of eyes, face, nails, skin, urine and stool, appearance
of network of veins with blue, yellow, green, and coppery color. If not treated
in time it gets easily suppurated. Virechana is advised but in weak
patients, Anuvasana and Niruhbasti with Ksheera is
advised. Eranda, panchatikta, Nishotha are given with different combinations of Virechana.
Virechana or Virechana after Baladhana and constant Ksheera-abhyas are Chikitsa
sutra of Pittodara[vi].
Pancreas
is referred as Agnyashay in ayurveda. There are eight types of Koshthanga
(visceral organs) described in ayurveda. Agnyashay is one of them. PachakaPitta
is assumed as the Dravya of Agni and Agnyashaya is the
container of Agni. When more Pachaka pitta accumulate in duodenum then
it induces reflex and activate zymogen to induce Shopha of Agnyashya
due to Usna-tikshna Gunas of Pitta can manifest Shopha.
Gall bladder slug and sphincter of oddi dysfunction/obstruction and
inflammation of pancreatic duct can be correlated with Sroto-sanga mentioned in
Ayurveda. So Pitta-shamana and Sroto-shodhana are the therapeutic
target in treatment of pancreatitis.
PRELIMINARY
DATA OF PATIENT
Age- 23 year
Sex- female
Date of admission – 01/12/2021
Date of discharge – 02/02/2022
CASE
DESCRIPTION
On
dated 1 December 2021, she came at our hospital, she had complain of vomiting
(after ate any type of food except coconut water) and lower abdomen pain. Then
she was admitted in our hospital.
History of present illness
•
Patient was healthy before 10 years.
Then, she had complaint of epigastric region pain and vomiting. So, she went to
gastroenterologist for her treatment. She had been admitted at hospital for iv
treatment for 8 days.
•
After every 6-8 months, she was admitted
in hospital for same complains.
•
She was diagnosed with acute
pancreatitis in 2018.
•
She
was diagnosed with antral gastritis and Malabsorption syndrome in July 2021.
•
She
was diagnosed with chronic pancreatitis in October 2021.
ON
EXAMINATION
• B.P.
– 118/76 mm hg
• P.R.-88
/min
• R.R.-
20/min
• Weight-
40 kg
Table 1:
|
Personal history |
|
|
Diet |
Vegetarian |
|
Appetite |
Normal |
|
Bowel |
1 time/day |
|
Sleep |
Normal |
|
Micturition |
5-6 time/day |
Table 2:
|
Dashvidha pariksha |
|
|
Prakriti |
Pitta-vata |
|
Vikruti |
Lakshna nimitta |
|
Sara
|
Rasa sara (madhyama) |
|
Samhanana |
Hina |
|
Pramana |
Hina |
|
Satmya |
Madhyama |
|
Aaharashakti |
Abhyavarana shakti : Hina Jaran shakti : Hina |
|
Vyayamshakti |
Hina |
|
Vaya |
Madhyama |
![]()
Samprapti
Nidana Sevana
Aaharaj- Katu,Amla-Lavan-Ushna-Teekshan-Vidahi
Viharaj-
Agni-Aatap Seven
Adhyashan &
Ajeernashan
(she ate too much pickle and oily spicy food )
Prakupitten
Vat-Shleshma Margavarodh
Unmarg(Vimarg-gaman)
Agni-nash
Pittodara
Table 3:
|
Samprati Ghataka |
|
|
Dosha |
Pitta pradhana
tridosha (kledaka kapha kshay, pachak pitta kshay, apana vayu pratiloma gati) |
|
Dushya |
Prana, Agni,
Apana sandusyUdaka, Rasa, Rakta ,Mamsa,Meda,Asthi,Majjja,Sukra |
|
Srotas |
Annavaha,
Udakavaha, Purishvaha, Rasavaha, Raktavaha, Swedavaha |
|
Udbhavasthana |
Aamashaya |
|
Adhisthana |
Sharira |
|
Vyktisthana |
Udara,
Agnasaya |
|
Agni |
Dhatvagni evam
Jatharagni Manda |
|
Srotodusti |
Sanga |
|
Sadhya-asadhyatva |
Kruchhsadhya |
|
Sama/nirama |
Nirama |
Table
4:Treatment
|
1/12/2021
to 1/2/2022 |
1.Shanshamani
vati- 2/2/2 2.Sudarshan
ghanvati- 2/2/2 3.Hingvashtak
churna-2 gm dhatriloha- 500mg muktasukti bhasma- 500mg 1 X 2 time 4.Tab.Sooktyn- 2/2/2 5.Tab.cytozen- 2/2/2 6.Tab.
Suv. Sootshekhar rasa- ½, ½, ½, ½ 7.Panch-karma – Kshirbasti (bindu prakshep) Water – 1 litre Milk -250 ml Guduchi churna -20 gm Vasa churna -20 gm Khadir churna -10 gm Kalmegh churna -20 gm Haridra churna -10 gm Lodhra churna -10 gm Punarnva churna -20 gm After 1 week
, added 10 ml gomutra. |
|
2/2/2022
to till now |
1.Aarogyavardhini
vati- 2/0/2 ( for 1 month ) 2.Sanshamani
vati- 2/0/2 3.Poonarnava
mandur- 2/0/2 4.Pathyadi
kwath-10 gm 1 X 2 time + kalmegh 5 gm
punarnava 5 gm Tab.Sooktyn- 2/2/2 Tab.cytozen- 2/2/2 Tab.
Suv. Sootshekhar rasa- ½, ½, ½, ½ |
RESULT
Patient did not take any contemporary medicine and she got completely relief through ayurvedic treatment. After 3rd day of treatment, improvement was seen in abdominal pain, nausea and vomiting. After 7 days of sansarjan krama, she could able to eat normal food. Kshirbasti holding time increase day by day. 26th kshirbasti holding time was 24 hour. After 2 month treatment patient had not any complaints.
Table 5:
|
No.
|
Symptoms
of chronic pancreatitis |
|
Duration
|
After
treatment |
|
1
|
Upper
abdominal pain |
Present
|
10
years(on & off ) |
Absent |
|
2
|
Abdominal
pain radiates to back |
Absent
|
- |
- |
|
3
|
Abdominal
pain that feels worse after eating |
Present
|
10
years |
Absent |
|
4
|
Nausea |
Present
|
10
years |
Absent |
|
5
|
Vomiting
|
Present
|
10
years |
Absent |
|
6
|
Weight
loss |
Present
|
Gradually
|
Absent |
|
7
|
Diarrhea
|
Absent
|
|
DISCUSSIONS
As
we understand that “Pittodara” is mainly caused by dominant localised
Pittadosha. Sequence of localised pitta dosha must be reviewed as per the
concept of Dhatugtatva of the disease mentioned in Jwara and Vatavyadhi
chikitsa. As per the general consideration each and every disease
penetrates/progresses into deeper tissue viz. Rasa, Rakta etc onward.
Malignancy is considered as Sukragatatva of the disease where regeneration
process of the body is completely disrupted. Fibrosis in the tissue is also a
type of Sukragtatva of the disease where body loose active specific cells of
group of cells or tissues. The present case is also considered the Sukragata
pathology of the pittodara because of chronicity of the disease as well as
severe imbalance in Agni at Dhatu level leading to excessive Dhatukshaya
condition in presence of pratiloma Vayu. The management of pittodara instructed
by Acharya Charaka is completely sufficient to check such condition of
Sukragata level of Pittodara.
When patient first visited our hospital,
she was not able to drink even normal water or take any kind of food article
since last 6 months except coconut water. She was too much anxious and in grief
when modern doctors advised her for surgery (partial pancreatomy).
She was given
Suvrna Sootshekar Rasa initially, in small dose to boost immunity and regulate
the function of vitiated Pittadosha. Along with this Deepana, Pachana, Tikta
and other Pittashamaka drugs given as mentioned above. As per the instruction by
acharya Charaka for weak pittodari, Tiktakshir vasti was planned to give
strength to the body and to revert the Pratiloma Vayu that was responsible for
Agnimandya, Aruchi, Hrillas & Chchhardi etc. On 3rd day of the
treatment, patient tried to take Mudagayusha etc. as per instruction but it
resulted nausea and vomiting on/off, Then classical Sansarjana krama started
and it responded very well because of Anulomana Karma shown by Kshirabasti
being given simountaneously.
After seven days
of sansarjana krama, she could take regular food. Day by day her appetite was
improved and her kshira basti holding time gradually increased.
Dhatugatatva of Pittodara
Dhatugatatva
concept well mentioned by Acharya Charaka in Jwara and vatavyadhi chikitsa. It
can be observed in each and every chronic disease. So as per this principle of
the pittodara progressed up to the level of sukradhatu where active pancreatic
cells became fibrosed and pancreas/body was unable to regenerate to fibrosed
cells. Hence consideration of pittodara can be justified very easily and the
result obtained with the use of kshir-basti, gold preparation and ubhay- prtyanik chikitsa confirms this.
Table 6:
|
|
Rasa |
Rakta |
Mamsa |
Meda |
Asthi |
Majja |
Sukra |
|
symptoms |
Aruchi |
Pittashay-shotha |
Weight loss |
Weight loss (Kaarshya) |
Calcification in pancreas |
Generalized
weakness |
Anartva |
|
Ashrdhha |
|
Pittashay-shotha |
plihavrudhhi |
|
bhram |
Fibrosis of pancreas |
|
|
|
|
Lymphnode enlargement |
|
|
|
|
CONCLUSION
Chronic
pancreatitis originated diabetes mellitus with precancerous and malabsorption
stage /jirna dhatugat pittodara can be managed effectively with the principle
of jirna pittodara in dhatugatatva from Suvarna sootshekhar rasa with other
vyadhi prtyanik chikitsa and tikta-kshir basti along with appropriate dietary
restriction are capable to treat this disease.
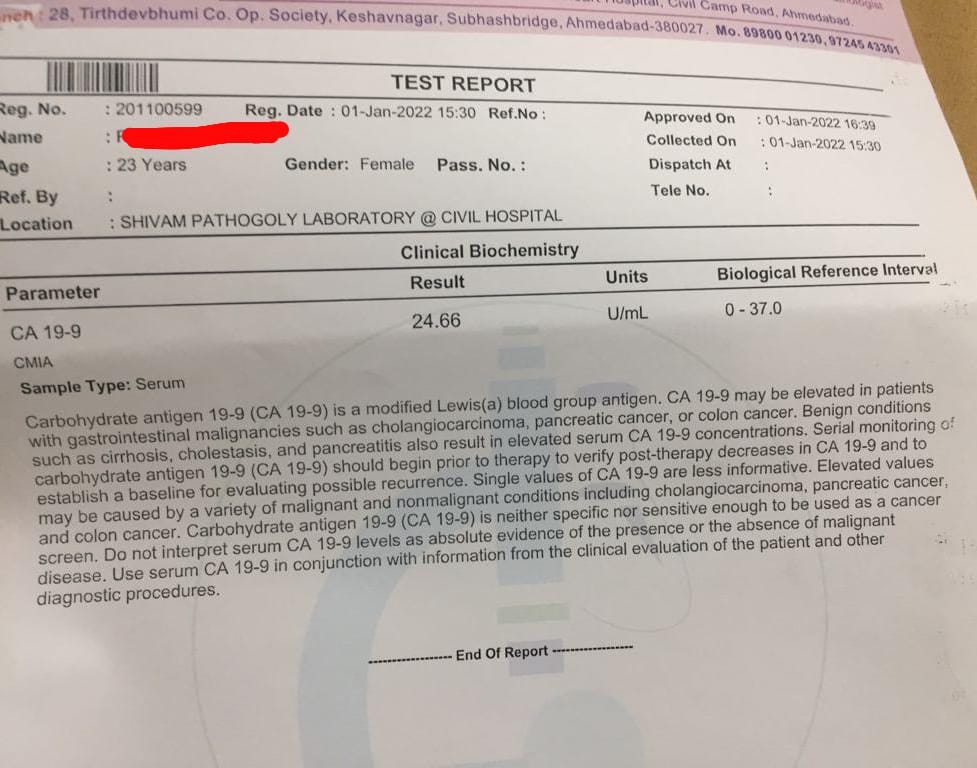
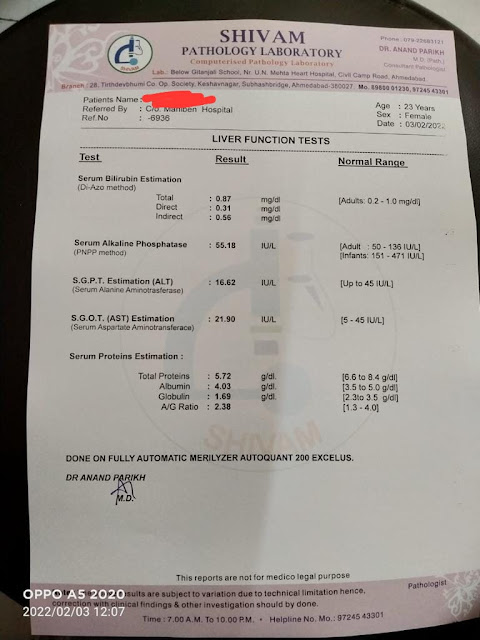
This patient had been
advised to go for partial pancreatomy because of high cancer marker CA 19/9,
while ayurvedic management not only reverted the CA 19/9 within the limit but
also CT-scan of Abdomen, USG of Abdomen, HbA1C and CBC proved the mark
improvement. That is perfect evidence to show the efficacy of management.
Table-7:
Investigation Summary
|
|
|
|
|
|
|
|
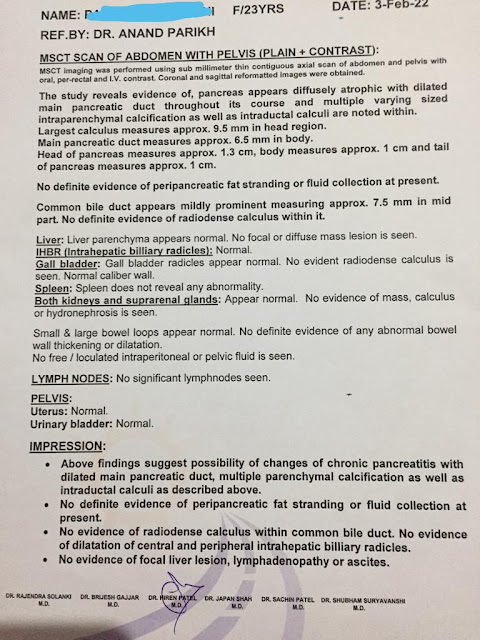
BEFORE TT 6/10/21 |
On 01/01/2022 |
On 3/2/22 |
28/04/2022 |
|
Chronic
pancretitis Largest
calculus 12.8 mm MPD size 8.3 CBD size 10 mm Fibrotic changes of duodenum wall Changes of para duodenal pancreatitis & reactive Lymphnodes |
- |
Chronic
pancretitis Largest
calculus 9.5 mm MPD size 6.5 CBD size 6.5
mm No evidence of Fibrotic changes of duodenum wall No evidence of paraduodenal pancreatitis &
reactive Lymphnodes |
- |
|
|
CA 19/9 |
58.52
U/mL (0-37) |
24.66
U/mL (0-37) |
- |
17.26
U/mL (0-37) |
|
HBA1C |
7.7 % (174 mg/dL) |
6.7 % (146 mg/dL) |
6.3 % (134
mg/dL) |
6.2 % (131.24
mg/dL) |
|
WBC count |
10250/ cmm |
8000 /cmm |
7100 /cmm |
6390 /cmm |
 |
REFERANCES
[i]Kleeff J, Whitcomb DC, Shimosegawa T, Esposito I, Lerch MM, Gress
T, et al. Chronic pancreatitis. Nat Rev Dis Primers
2017;3:17060.
[ii]The National Pancreas Foundation. Chronic Pancreatitis; 2019. Available
from: https://pancreasfoundation.org/patient-information/chronic-pancreatitis/. [Last accessed on 2020 Jul 07].
[iii]Banks PA, Conwell DL, Toskes PP. The management of acute and chronic pancreatitis. Gastroenterol Hepatol 2016;6:1-16.
[iv]Barry K. Chronic pancreatitis: Diagnosis and treatment. Am Fam Physician
2018;97:385-93.
[v]Jitesh M & Uma Venugopal. Ayurvedic approach to chronic Pancreatitis: A case report, Int J Sci Res 2016;5(9):564-66.
[vi]Sharma RK, Dash B: Agnivesha’s Caraka Samhita. Text with English Translation. Volume 3. 4th edition. Varanasi: Chowkhamba Sanskrit Series Office; 2000:13(38):521.
***********************************************************************************************************************************************************************************
Presented by:-
*Vd. NIRALI S. THACKER,
Final year P.G.
Upgraded P.G. Dept. of Kayachikitsa, Govt. Akhndanand Ayurveda College, Ahmedabad, Gujarat, India.
**Vd. SURENDRA A. SONI,
M.D., PhD (KC),
Professor & Head,
Upgraded P.G. Dept. of Kayachikitsa,
Govt. Akhndanand Ayurveda College, Ahmedabad, Gujarat, India.



















Comments
Post a Comment